When I entered rehab at 23, I learned that trauma was a thread woven into most addiction stories. Many people in my program described horrific neglect or maltreatment, including sexual abuse, they had experienced as children. Still, few seemed to realize how traumatizing those things had been. The traces of trauma in my own life were not then obvious to me, either, perhaps because my parents had suffered so much worse. Now, however, I can see that some of my extreme sensitivities, such as my fear of crowds and enclosures, eerily reflect my father’s story.
When my father was a kindergartner in Hungary, he and his mother were crushed among thousands of starving concentration-camp victims on a train bound for Auschwitz. It was abandoned by the Nazis as the Allies took control in 1944. My father didn’t speak for a year afterward and struggled with depression for most of his life. My mother’s trauma was more ordinary: she lost her mother to cancer in early adolescence. They were loving parents, but I grew up feeling unworthy because nothing I did seemed good enough. Easily overwhelmed by sensory and social encounters, I cried often, which led to my being bullied in school.
As a teen, I found that drugs—first marijuana, then psychedelics and, it being the 1980s, cocaine—made it easier for me to connect socially. But heroin, which made me feel calm and satisfied and safe, was my favorite. By 1986 I was injecting daily and had to leave Columbia University. Two years later, when I weighed 80 pounds and had already made many failed attempts to quit on my own, I finally recognized that shooting coke and heroin up to 40 times a day definitely meant I was addicted and needed help.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Like most rehabs even now, the one I attended was based on the 12-step program of Alcoholics Anonymous (AA). The organization was founded in 1935 by a stockbroker and a doctor who believed their own addiction to alcohol had derived from “defects of character,” such as being selfish and avoiding responsibility. The main active ingredient of 12-step programs, which now exist for practically every type of addiction—from cocaine to overeating to gambling—seems to be the social support of group meetings. These have helped millions of people, including me. But some of the program’s aspects have harmed people who were told that strict adherence to the rules was the only way to recover. One particularly problematic teaching is that recovery requires addicted people to see their misbehavior as the cause of their problems—rather than encouraging them to understand why they might have been especially prone to seeking solace in substances.
Growing awareness of how addiction and trauma are intertwined has birthed a new generation of treatment strategies.
In recent decades a body of research has established that adverse childhood experiences are critical in the development of substance addictions. A 2021 review found that more than 40 percent of people with opioid addiction reported some type of childhood abuse or neglect, and 41 percent of women had been subjected to childhood sexual abuse, much higher than the rate for the general population. A different study showed that among those with any type of addiction, at least 85 percent have had at least one adverse childhood experience, with each additional experience raising the risk. The link is most pronounced among those diagnosed with post-traumatic stress disorder (PTSD), characterized by flashbacks and other psychological disturbances that can develop in response to a shocking or terrifying event. Among people treated for any substance addiction, one third have active PTSD—and among those with PTSD, 58 percent have had problems with substance use.
This awareness of how addiction and trauma are intimately intertwined has birthed a new generation of treatment strategies that simultaneously address both issues. So far they have been tested mostly for people with both PTSD and addiction—and they reinforce the idea that the trauma drives the substance use. “What we see is remarkable,” says Teresa Lopez-Castro, an associate professor of psychology at the City College of New York. “When the PTSD symptoms go down, the substance-use-disorder problems will go down, but the opposite doesn’t happen that frequently.” My own examination of addiction over the past four decades has convinced me that trauma-informed care is superior to the traditional methods, which often seek to erase a patient’s autonomy and thereby risk compounding existing wounds or inflicting fresh trauma.
The suffering that predisposes someone to addiction doesn’t have to be overt. As in my case, it can be as seemingly mundane as being raised by depressed parents or being bullied in school. Other circumstances that increase vulnerability include having addicted or mentally ill parents; witnessing violence; losing a parent; or experiencing a life-threatening illness, accident, conflict or disaster. A study of the entire Swedish population found that undergoing just one of these potentially traumatizing experiences may double the risk for substance use disorders.
Brain imaging and other techniques have teased out the neurological pathways entwining trauma with addiction. Both experiences change the brain’s reward systems, which motivate people to seek evolutionary essentials such as food, water, sex—and, crucially, safety. Brain signals are complicated, however, and many seemingly separate “systems” share the same circuitry. Systems that predict reward or punishment are deeply intertwined with the modulation of stress: many of the same neurotransmitters and brain regions involved in motivating us to seek pleasure and satiety also help to keep us safe.
Dopamine, for example, drives us to seek sources of pleasure linked to survival and reproduction and also to avoid threats. The neurotransmitter acts on the striatum and the prefrontal cortex, both of which are in the forebrain, and helps us predict whether an experience will be rewarding or upsetting. It does so by creating a feeling of “wanting”—either to get more pleasure or to escape from pain. And during scary or stressful experiences, endogenous, or self-generated, opioids known as endorphins and enkephalins are released in the brain. These are guided by hormones from the adrenal and pituitary glands as part of the classic stress-response system, to ease pain and facilitate escape. These opioids also make food, sex and socializing feel good, causing a feeling of “liking” something or someone and of satiety and comfort.
Growing up in a threatening and stressful environment can undermine this circuitry. Studies in both humans and animals show that adversity in childhood alters the regulation of stress hormones such as cortisol. These hormones, released during prolonged or acute stress, change brain regions such as the amygdala, which is activated by strong emotions, especially fear and distress. Stress in early life also alters the nucleus accumbens, a part of the striatum that is key to addiction: it makes us want more of what feels good. Memory areas such as the hippocampus are also profoundly affected, making some memories too strong and others too weak. “Our reward system and our stress system become attuned to trying to meet the needs of reducing threat,” Lopez-Castro says.
Research shows that people who have experienced childhood trauma are more aware of and sensitive to signs of a potential threat. Someone whose father was always raging, for example, may interpret even neutral facial expressions as angry. Moreover, rapid responses are often necessary when someone is under threat. But repeating them strengthens emotional brain regions and reduces the influence of the prefrontal cortex, which puts the brakes on impulsive actions. Living with fear and anxiety can therefore impair impulse control—leaving some children more likely to both see threat where it isn’t and react to it rapidly, with little consideration of consequences. Such responsiveness can be lifesaving in threatening environments. But it also can be detrimental when impulsive reactions interfere with the child’s ability to learn that a situation is in fact safe and thereby lead to behaviors that others perceive as aggressive.
Even after the trauma has ended, these brain changes remain. “Our ability to sort of shift to thinking, ‘Oh, everything’s safe now’ is very much compromised,” Lopez-Castro says. This impairment can lead to a person prioritizing immediate relief—by, for example, taking drugs—over planning a future that seems either uncertain or unlikely to be better than the present.
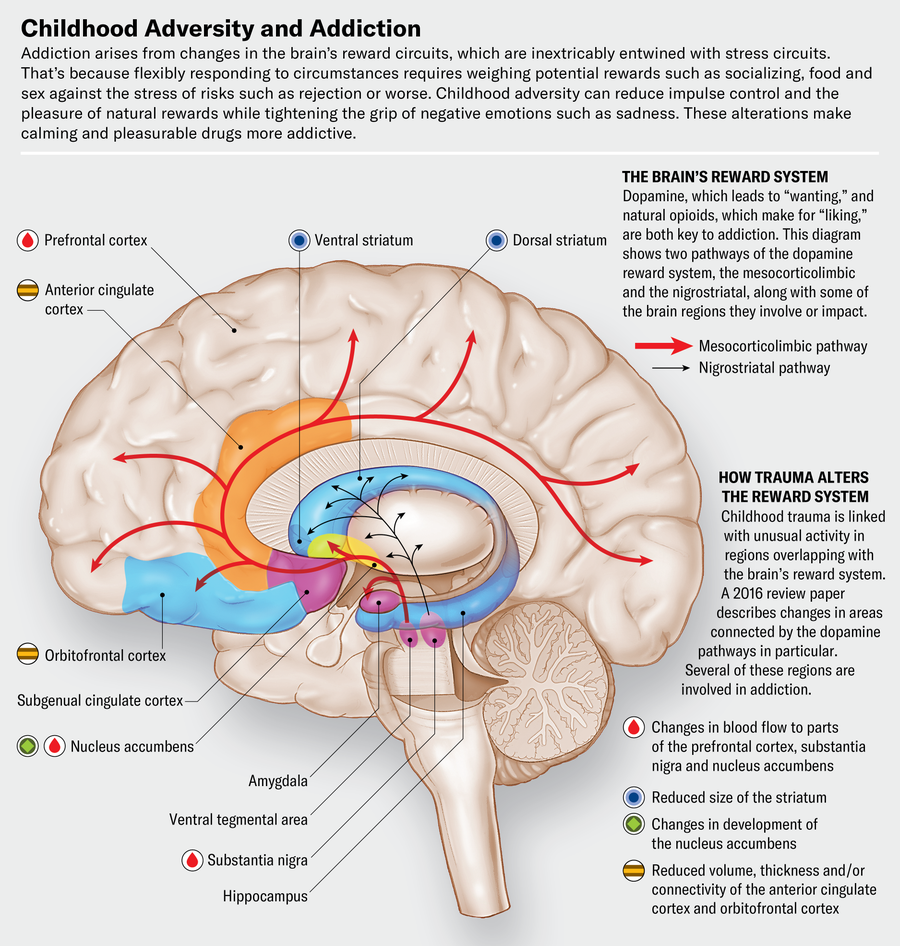
Body Scientific; Source: “The Effects of Childhood Maltreatment on Brain Structure, Function and Connectivity,” by Martin H. Teicher et al., in Nature Reviews Neuroscience, Vol. 17; September 2016 (reference)
Another possible consequence of early-life adversity is anhedonia, an inability to experience pleasure, which in turn can suppress motivation. My own experience of it was a sense of dread and dullness of mood that I couldn’t verbalize but that made me constantly uncomfortable in my own skin. This symptom is a common characteristic of depression and, unsurprisingly, makes people vulnerable to misusing substances that promise relief.
“When trauma happens early in life, it really kind of destabilizes us—but we adapt,” Lopez-Castro explains. The relevant adaptations in the reward and stress systems can help people survive, but they also can take a toll on emotion regulation. Overall, severe early stress can create a general sense of dread and pleasurelessness—so if traumatized kids are exposed to drugs that amplify dopamine or activate the brain’s own opioid systems, they are highly susceptible to becoming addicted because the drugs offer the excitement and comfort they otherwise lack.
At the same time, genetics affects addiction risk by setting defaults. Some infants are more easily distressed, for example, whereas others have calm temperaments. These variations reflect the responsiveness and resilience of the stress and reward systems. Roughly half the risk for substance use disorders is genetically determined, but the way this predisposition plays out is extremely varied. Some genes put people at risk via personality traits such as being prone to thrill-seeking or having difficulties with impulse control; others work by causing difficulty focusing, low moods or anxiety. Yet others, such as the genes related to the metabolism of alcohol, alter the risks associated with particular substances.
Traumatic stress is most often what tips these traits and tendencies into pathologies or disabilities. Addiction often results from attempts to self-medicate the symptoms—which is why treating the underlying trauma can be essential to a cure.
Michael, a veteran in his 30s who has struggled with both PTSD and addiction, understands all too well how they are connected. (Names have been changed for privacy.) Fortunately, he was able to get both treated simultaneously as part of a study led by Sudie Back, professor and director of addiction sciences at the Medical University of South Carolina.
The treatment included a psychotherapy called COPE, which stands for “concurrent treatment of PTSD and substance use disorders using prolonged exposure.” On its own, COPE has been found to be safe and effective in multiple clinical trials. The study Michael enrolled in tested whether adding the social-bonding hormone oxytocin could improve outcomes. Such combined therapies for co-occurring disorders offer a glimpse of what better care could look like in the future.
Michael was raised on a prison farm, where his father worked in corrections. From an early age he was abused by an older relative who beat him and persistently threatened him with sexual assault. He joined the air force just after high school, and in Afghanistan he volunteered for risky assignments. “I was 18 and wanted stories to tell,” he says. The first time his unit got attacked, though, he slept through the first few minutes, which led him to start taking stimulants: he never wanted to be caught off guard again.
Combat and witnessing so much suffering and death caused PTSD. (Childhood abuse seems to increase the risk of PTSD developing later in life in response to acute stressors.) At the time, Michael says, everything felt “surreal,” and he wasn’t really processing anything emotionally. He was also drinking and taking large quantities of “speed”—stimulants such as amphetamines that promote wakefulness and, in large doses, can cause paranoia. “People in my chain of command were noticing that I had a lot of issues with anger,” he says. Recognizing his problem with stimulants, Michael quit taking them in 2007 and started counseling to deal with his intense rage, a common symptom of PTSD. Returning home after six years of service, he had difficulty adjusting and was drinking heavily. He enrolled in the trial in 2023.
COPE involves 12 weekly 90-minute sessions led by a trained therapist. Because drug cravings are often driven by stress, COPE teaches better emotional regulation and thereby addresses PTSD and addiction simultaneously. Participants in the program are asked to recount their traumatic experiences repeatedly in a safe place, which helps them manage stressful memories and stop avoiding environments and experiences that can trigger them. They are also gradually exposed to increasingly challenging situations that they would typically avoid, at a pace they control.
Brain changes induced by adversity can lead to a person prioritizing immediate relief over planning for an uncertain future.
“At the heart of trauma—and trauma-related issues—is avoidance,” Lopez-Castro says. By replacing avoidance with approach, exposure therapy retrains the brain to recognize safety. Over time this strategy increases both the ability to tolerate stress and the capacity to stay calm in situations that evoke the fear, grief or anger associated with past traumas, which is essential to recovering from both PTSD and addiction. Because alcohol and other drugs are often craved during and used to cope with strong emotions, COPE also teaches alternative ways of managing distress such as breathing techniques and seeking support from others.
Further, because trauma is marked by a sense of helplessness in the face of potential annihilation, recovery from it requires maximizing the patient’s sense of control, security and autonomy. Toward this end, therapy needs to be highly structured and predictable so the patient knows what to expect and can pull back if it becomes overwhelming. “We talk to them about the rationale, which is so important,” Back says.
Many addiction-treatment programs, unfortunately, view questions about process as resistance to recovery. Newcomers to 12-step programs are often told to “shut up and listen” because “your best thinking got you here.” This dismissive approach can generate mistrust, especially if patients perceive that counselors are being punitive rather than helpful when pushing them to confront their fears. In contrast, effective trauma and addiction therapists explain exactly why they are going to ask patients to face the painful situations they most seek to escape—and how this will diminish the power of these memories when done slowly and with a measured and controllable escalation of intensity.
Traumatic memories are often stored differently in the brain, which may account for why people with PTSD experience them as “flashbacks” and feel as though they are reexperiencing terror here and now. The therapeutic process in COPE can transform the patient’s recollection of past traumas from fully reexperiencing them into simply telling a story of what happened—and may help the brain process these memories more typically. As Back has noted, the COPE program reduces PTSD symptoms—and that in turn cuts drug craving and use. Simply stopping the drugs doesn’t help the underlying issues and can, in fact, exacerbate symptoms.
Another prominent commonality between addiction and PTSD is that maintaining strong social connections is usually essential to lasting recovery because healthy relationships are physiologically fundamental to stress relief. This dynamic begins in infancy: babies literally cannot modulate their stress system without nurturing touch from caregivers, which releases endogenous opioids and oxytocin, creating a sense of comfort and safety. In normal development, oxytocin may link this stress relief in the presence of loved ones to the activation of the opioid system. Both substances are released when parents soothe their children, creating an association between the parent and comfort. Later, when Mom “kisses the boo-boo to make it better,” this gesture triggers endorphins to relieve the pain and stop the tears.
In earlier research, Back and her colleagues found that the therapeutic bond between patient and therapist is a leading determinant of recovery—so they thought adding oxytocin might improve this connection. One study by the group of people who had PTSD without addiction showed that oxytocin accelerated positive change. The new study, which included those who had PTSD with addiction, hasn’t been completed or unblinded, so Michael doesn’t know whether he got the hormone or a placebo. But he does know that he got better.
“I think it was really just being able to get some things out that I had put to the side and then just the way the whole process went,” Michael says, describing what helped him most. He stresses that his relationship with his therapist was crucial, calling her “very personable” and “very understanding.” The repetition and emotional safety helped him make sense of his experiences and put them more firmly behind him. He is now able to use alcohol moderately without returning to his prior compulsive drinking.
Another promising approach that can be combined with addiction treatment is known as cognitive processing therapy (CPT). This treatment focuses on minimizing patients’ distorted thoughts and self-concept rather than exposing and taming the traumatic memories themselves. It can be especially useful for people whose fear of their own traumatic memories prevents them from revisiting the experiences—the biggest obstacle to the success of COPE and other exposure therapies.
Sandra started drinking with friends when she was 15. “I remember feeling anxious from a really early age,” she says. “It just alleviated that feeling for me.” Over the next few years she became dependent on alcohol and, later, ketamine, which she began using at raves.
In her early 20s Sandra had just started treatment for her substance use disorder at a program in New York City called the Center for Motivation and Change when she was held hostage and sexually attacked by a boyfriend she was trying to break up with. She received CPT after a coach connected with that organization helped her have him arrested and get a restraining order.
Sandra says the treatment targeted “false beliefs or core ideas that you’ve had about the world and other people due to the trauma.” She gives several examples: “A main one was, like, I’ll never be a good girlfriend or, like, girlfriend material. I’ll never find happiness. Or I’ll never feel safe again.”
Her ex had told her repeatedly that he was the only one who would ever want her. CPT helps patients reality-test these ideas and reject the overgeneralizations and catastrophic thinking they represent. When these hyperbolic thoughts are expressed in the safety of therapy, their power is diminished, and healthier ways of seeing can start to replace them. Sandra initially attempted to moderate her use of alcohol and other drugs but ultimately decided on abstinence.
Trauma is so prevalent among people with addiction that all treatment programs need to be prepared to address it.
She’s now been sober for more than a year but has a mixed relationship with 12-step programs, which she had tried at various times and now uses selectively. She had to drop one AA sponsor, or mentor, who tried to engage her in a harmful version of the fourth step, in which people take “moral inventory” to look at the character defects the program sees as underlying addiction. The written version of this step asks participants to focus on accepting a role in major events in their lives so that they can take responsibility for their actions. In the course of this effort, Sandra’s sponsor asked her to look for her part in having been assaulted. “I just did not agree,” she says, and she fired the sponsor. For victims of trauma, believing that being raped or abused was somehow their fault is profoundly damaging—and is one of the beliefs that both COPE and CPT aim to change, not reinforce. These days Sandra attends certain AA meetings for social support but does not engage with those who push problematic ideas about the steps.
My own experience of the fourth step was much more positive, largely because the person I worked with recognized that like many other women struggling with addiction, I had a bigger problem with hating and blaming myself than I did with trying to avoid accountability.
Treatment providers have tried to move away from this “tough love” approach in recent years. But it is hard to eliminate it because many 12-steppers employed as counselors believe that what worked for them should work for everyone. Worse, many facilities, often called “therapeutic communities,” are modeled on a defunct cult called Synanon that was seen as having found the first real cure for heroin addiction. Synanon’s leadership believed that voluntarily working the steps was too soft and turned the method into a coercive one, using confrontation, humiliation and emotional attacks as ways to force change. (AA—a voluntary, self-governed group—takes no official position on treatment policies and practice, so it cannot address misuse of its program.)
Nzinga Harrison is co-founder and chief medical officer of Eleanor Health, which provides evidence-based online and outpatient addiction and mental health care to around 30,000 people in seven U.S. states. The overwhelming majority of these patients have had prior negative experience with treatment, she says. “They experienced traumas in their early life, and then they go into treatment, and the treatment itself is traumatic, reinforcing abandonment, devaluing them.”
Lopez-Castro adds that “the shaming that has been so much a part of their experience of being traumatized is then evoked in [treatment] settings where they’re told, ‘You are weak, worthless.’” She has conducted interviews with people with PTSD who were addicted to cocaine and heroin and were receiving clean needles from a program intended to reduce the health risks associated with syringe use. Many, especially the older ones, reported that their prior experience of treatment was being screamed at or being made to scrub floors with toothbrushes and wear dunce caps. “It has been really brutal for them,” she says, “and these were their formative experiences of treatment.”
Lopez-Castro is starting work on a study that will look at whether providing trauma-informed, empathetic care to people who inject drugs can help participants reduce harms associated with drug use. This effort is based on insight from harm-reduction therapists, who have found that some traumatized people cannot even start to change their drug use patterns without first learning alternative methods to manage trauma symptoms.
PTSD and addiction also can be addressed through approaches that increase neuroplasticity, which is the brain’s ability to change and adapt in response to experience. Neuroplasticity varies over the lifetime. Early childhood and adolescence are known as sensitive or critical periods when the brain is most capable of learning rapidly and altering its trajectory in both positive and negative ways. If adverse experiences occur during these times, they can hardwire dysfunctional behavior patterns, making them difficult to change.
Treatments that alter plasticity are therefore likely to be helpful, as long as they are used under conditions where people can safely learn healthier strategies for organizing the way they think and act. Everything currently known to have antidepressant effects—from medications such as fluoxetine (Prozac) to exercise—increases plasticity as well and might augment other therapies for PTSD and addiction.
Intriguingly, psychedelic drugs such as LSD and psilocybin mushrooms have recently been found to rapidly increase plasticity and may act by restoring the plasticity associated with critical periods. Researchers are now studying these substances to separately treat PTSD and various addictions, and early clinical trials with MDMA, known colloquially as “ecstasy” or “molly,” suggest promising results. MDMA not only increases neuroplasticity but also prompts the release of oxytocin, which may account for why people often describe their experience on the drug as one of feeling connected, empathetic and loving. This social specificity may make it especially helpful for people with PTSD and addictions.
One clinical trial of people with moderate to severe PTSD, published in 2023 in Nature Medicine, found that 46 percent of participants had complete remission of symptoms with therapy plus MDMA, compared with 21 percent in the group that received the same therapy plus a placebo. Researchers in Australia are now studying the combination of COPE and MDMA for people with PTSD and alcohol use disorder. Other studies of various psychedelics to treat addiction and PTSD, separately or simultaneously, are also underway. The U.S. Food and Drug Administration has designated MDMA, LSD and psilocybin as potential “breakthrough” medications, which puts them on a faster track toward approval. In early August, however, the FDA rejected MDMA-assisted therapy for PTSD, asking for another phase 3 trial to further assess benefits and safety.
Both addiction and PTSD are complex conditions, and it is unlikely that any single approach will work for everyone. But there are now more options than ever, which should bring greater odds of recovery. Evidence-based approaches such as COPE and CPT need to be made available more widely, and people with addiction must be empowered to choose the therapies that best align with their needs. Because traumatic experience is so prevalent among people with addiction, all treatment programs need to be prepared to address it—and to ensure that treatment at least does no harm.
I am lucky to have avoided the most traumatic types of treatment when I was desperate and vulnerable. Although I was still subjected to some questionable practices, such as being treated in an authoritarian setting, I was ultimately able, as one highly useful AA slogan puts it, to “take what I like and leave the rest.” Making addiction treatment more trauma-informed and compassionate is not only the right thing to do, it’s the easiest way to rapidly improve outcomes and to get people to welcome much needed care.


































